the case.
It’s night shift & you’ve received handover of an entire department. You plug on and start chipping away at the waiting-list that doesn’t seem ever get any shorter….
At 3am your nursing staff alert you to an 11 year old female who just isn’t getting any better. She was admitted under Paediatrics on the evening shift with 24 hours of vomiting (no diarrhoea) & had failed her trial of fluid. Whilst she is waiting for a paediatric ward bed she has continued to vomit a further 8-10 times and is complaining of severe epigastric pain. She had used up all her available antiemetics and analgesics on her medication chart…
She looks miserable, crying in pain and clutching at her abdomen. She is slightly tachycardic (otherwise normal observations). Her abdomen is non-distended but exquisitely tender with percussion tenderness and rebound. She has reduced bowels sounds. There is a scar in her RIF indicating a previous open appendicectomy ( ~18 months earlier).
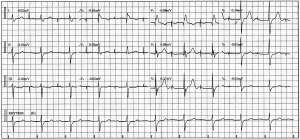
You review her bloods (WCC 16, otherwise unremarkable) and her urinalysis is normal.
Despite further boluses of morphine, she continues to vomit and complain of severe pain….so, you order an abdominal xray.

What’s going on here ?
What are you going to do now ??
Continue reading →